WHAT IS TRANSJUGULAR BIOPSY?
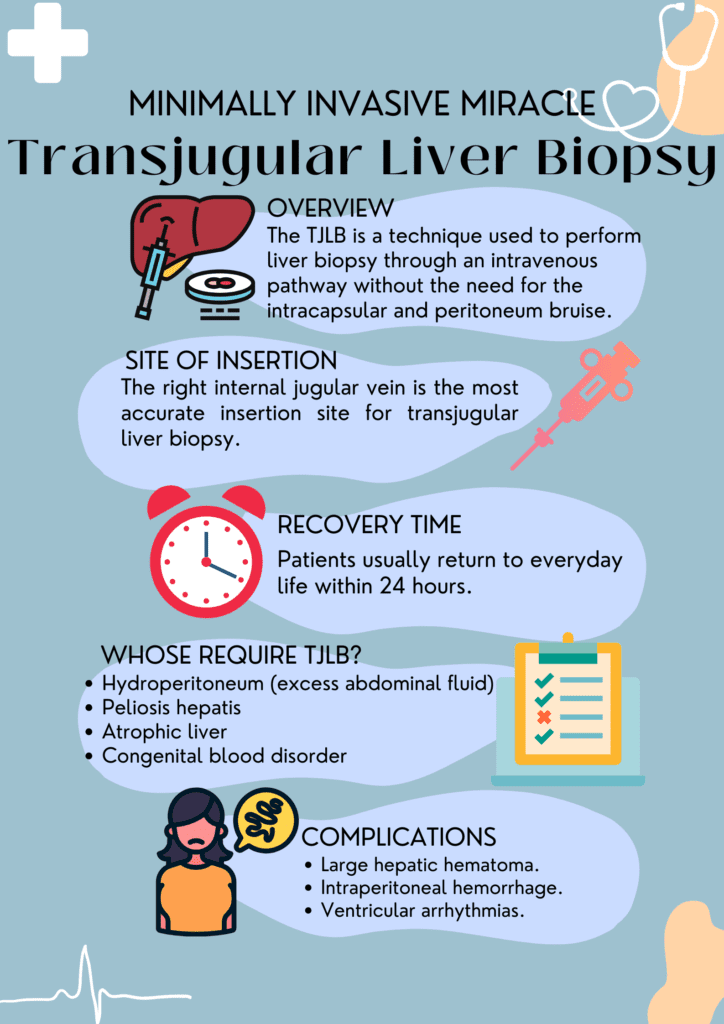
The transjugular biopsy is an emerging diagnostic technique in the medical sciences used to perform liver biopsy without the need of the intracapsular and peritoneum bruise.
The transjugular biopsy uses the concept of the intravenous pathway to examine without obstructing the hepatic tissues of the liver. Through an intravenous perspective, the biopsy-associated needle is inserted into the hepatic vein to reach the hepatocyte and visualize its crystal clear picture to the health care.
WHY LIVER BIOPSIES ARE IMPORTANT?
A liver biopsy is the most accurate method of evaluating and visualizing all acute and chronic liver disorders.
This technique has transformed how we diagnose liver conditions, offering a safer and more effective approach to a critical aspect of healthcare.
WHAT IS THE PURPOSE OF THE ARTICLE?
In this article, we will explore the world of transjugular liver biopsies, shedding light on what it is and why it’s making waves in the medical community.
And also provide some essential information regarding the process.
WHAT ARE THE INDICATIONS FOR TRANSJUGULAR BIOPSY?
The need for transjugular liver biopsy always depends upon the current health status of the patient, the disease progression, and associated complications. Some other factors which should consider the healthcare provider to prescribe the procedure are:
When Traditional Liver Biopsies Fall Short:
It is recommended to patients who previously underwent other types of liver biopsies like untargeted percutaneous liver biopsy and cannot get a clear view of the ongoing hepatic disorder.
For those which are contraindicated to percutaneous liver biopsy or have failed liver biopsy
Patients Who Require Transjugular Biopsies:
This diagnostic technique is suitable for patients suffering with
- Coagulopathy (high PPT)
- Thrombocytopenia (low Platelet count)
- Congenital blood disorders
- Hydroperitoneum (excess abdominal fluid)
- Peliosis hepatis
- Atrophic liver
- Chronic renal insufficiency
- Acute liver failure
- Portal hypertension
- Obesity
- Liver transplant
- Hepatic stent (transjugular intrahepatic portosystemic shunt procedure)
Advantages of Transjugular Biopsies:
- One of the most essential advantages of transjugular liver biopsy is that it reduces the risk of bleeding, which could be a life-threatening complication in patients with clotting disorders.
- The bleeding occurs because a biopsy needle will eventually drain into the hepatic veins as the capsule of Glisson is not punctured, which also minimizes the chances of potential blood loss.
- This technique also provides valuable clinical knowledge along with the guiding therapies in patients associated with portal hypertension by using the hemodynamic evaluation of the portal and systemic venous system.
WHAT ARE THE CONTRAINDICATIONS FOR TJLB?
- Although there is no special contraindication for the transjugular liver biopsy, it is recommended to consider the issues of coagulopathy until further proceeding to the process.
- Another comparative caution associated with the Tjlb is the lack of appropriate venous admittance and biopsy associated with the focal hepatic injury.
- Thrombosis of the hepatic vein, hydatid cyst, and cholangitis are also factors.
WHAT IS THE MOST ACCURATE SITE OF INSERTION FOR TRANSJUGULAR LIVER BIOPSY?
The right internal jugular vein is the most accurate insertion site for transjugular liver biopsy. However, if it is not assessable, the left internal jugular or femoral vein acts as a substitute site for biopsy.
THE TRANSJUGULAR LIVER BIOPSY PROCEDURE:
Pre-Procedure Preparation:
Before initiating the procedure, written, signed, and informed consent, which explains every detail to the patient regarding the process, the potential consequences, and the risks and complications.
4 to 6 hours of fasting before the process is recommended to minimize the risk of aspiration.
An abdomen ultrasound assesses the liver size, identifies any focal lesions, and assesses hepatic veins.
Sedation and Anesthesia:
The procedure is performed under local anesthesia along with sedative analgesics.
The Transjugular Approach:
- The patient is lying in the supine position on the table with the neck exposed and the head turned far from the location of the venous assessment.
- Ultrasonography is required for safety and to reduce complications such as puncture of pneumothorax and assessment of the obstruction status of the veins.
- The skin of the neck is prepared with an aseptic solution to disinfect the area and local anesthesia (lignocaine) intradermally and subcutaneously.
- A point is marked 3 to 5 cm above the clavicle to assess the right internal jugular vein to puncture. The right internal jugular vein is considered an ideal site for the hole as it provides direct access to the superior vena cava, inferior vena cava, and hepatic vein.
- Monitoring BP, ECG, and Pulse oximeter throughout the process is necessary.
- The right internal jugular vein is punctured under the guidance of USG using an 18G metal needle having a plastic cannula. A syringe must be attached to the hand for the aspiration of blood and to minimize the risk of air embolism. Aspiration of blood in the needle will confirm the puncture of the internal jugular vein.
- A suitable wire guide (0.035 inches for 18G) is passed across the needle when the vein is punctured.
- The wire, along with the multipurpose 5-fr catheter and a guide wire (0.035inch), is now required to pass across the superior vena cava toward the right atrium and then move to the inferior vena cava and finally into the right hepatic vein.
- During the transition toward the right atrium, arrhythmias will be noticed. These are usually transient and go away once the catheter moves toward the inferior vena cava.
- The Valsalva technique (breathing) is used to dilate the hepatic vein and quickly assess it. The right hepatic vein is considered a biopsy start point to ensure deep insertion, far from the liver capsule.
- Now, the catheter is advanced with the stiffening cannula 7F sheath, providing support and guidance to the Quick-Core biopsy needle.
- The Quick-Core needle is prepared outside and administered into the stiffening cannula when the cannula reaches at least the middle of the proper hepatic artery. This needle is responsible for extracting the hepatic parenchyma.
- Breath-holding is necessary during the biopsy to minimize the risk of hepatic injury through the needle.
- Usually, three samples are obtained through biopsy, two from the peripheral side and one from a relatively centralized area. The needle is pulled out from the stiffening cannula, and the sample is collected.
- Immediately after the biopsy, the hepatic venogram is performed to check the extravasation in the peritoneal cavity. Manual compression for about 10 minutes is recommended at the puncture site to obtain homeostasis.
Post-Procedure Care:
- After the biopsy process, the patient must remain in the sitting position for at least 6 hours.
- Vital parameters must be monitored.
WHAT ARE THE COMPLICATIONS ASSOCIATED TO TRANSJUGULAR LIVER BIOPSY?
The complications associated to the Transjugular Liver Biopsy includes:
Major Complications:
- Large hepatic hematoma.
- Intraperitoneal hemorrhage.
- Ventricular arrhythmias.
- Cholangitis.
Minor Complications:
- Neck pain.
- Hematoma.
- Bleeding.
- Carotid puncture.
- Allergic reactions.
- Dysphonia.
IS TRANSJUGULAR LIVER BIOPSY SAFE?
The TJLB possesses great effectiveness, highly bearable, less invasive and potentially safer procedures. It is practicable multiple times in the same patient and in severely ill patients with intense bleeding disorders with minimal rate of complications.
WHAT ARE THE RISKS OF TRANSJUGULAR LIVER BIOPSY?
During the sample extraction, the significant risk of transjugular liver biopsy is intraperitoneal bleeding and the liver capsule (Glisson’s) perforation.
WHAT IS TJLB RECOVERY TIME?
Patients usually return to everyday life within 24 hours.
TRANSJUGULAR LIVER BIOPSY AND PAEDIATRICS:
- Although liver biopsy is a favorable diagnostic tool for evaluating liver-associated disorders, at the same time, this procedure is invasive. Still, it contributes to the staging and etiological diagnosis of liver diseases.
- TJLB associated with pediatrics shows an intense technical success rate along with low complications.
- It is proven that the TJLB is an effective tool for disease detection and post-procedure consequences, specifically in patients with ongoing bleeding disorders and hydroperitoneum, where traditional percutaneous liver biopsy creates a risk factor.
- It is also suggested that the TJLB, along with the biopsy needle, is considered a safer and more appropriate method for the histological study of liver specimens in those pediatric patients who undergo left lobe or lateral segment liver transplant.
CONCLUSION:
In a world where medical procedures can be intimidating, transjugular biopsies are a breath of fresh air for those with liver problems. They’re safer, more comfortable, and can provide crucial information for treatment decisions. With ongoing research and improvements, this technique is set to become even better in the future.
4 thoughts on ““Transjugular Biopsy: A Minimally Invasive Miracle””