Introduction:
When it begins to diagnose and treat medical conditions, precision is critical. One remarkable tool that has been making waves in the world of urology is “Blue light Cystoscopy.” This article will demystify this innovative procedure and explore how it changes the game in diagnosing and treating bladder problems.
What is Cystoscopy?
- Cystoscopy, in simple terms, is a medical procedure, a type of bladder biopsy that involves examining the inside of the bladder, especially examining and sometimes surgically removing bladder tumors.
- The procedure is done by inserting a thin tube-like instrument with a camera lens on either side, known as a cystoscope.
- The cystoscope has a telescope or microscope used to magnify the inside image.
- In simple cystoscopy, usually a white-light camera is used.
What is Bluelight Cystoscopy?
- So, what makes it different from the traditional cystoscopy? Well, it’s all about the light. Instead of regular white light, Bluelight Cystoscopy uses a special blue light, making a world of difference in what can be spotted inside the bladder. This advancement has proven to be particularly important in the field of urology.
- Blue light cystoscopy is the latest and FDA-approved technology to detect and examine urinary bladder tumors more efficiently.
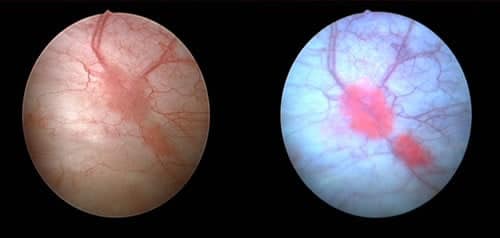
- This technique is also known as Cysview®. This procedure combines white light and blue light with the unique dye known as Cysview®.
What is Cysview®?
- Cysview®(hexaminolevulinate HCl) is a type of contrasting dye solution absorbed by the rapidly growing cells of the bladder (which might be suspect of a malignant tumor). It shows pinkish-red or red coloration when exposed to blue light.
What are the benefits of blue light cystoscopy?
- Bluelight Cystoscopy, often abbreviated as BLC, is a unique variation of this procedure that uses blue light to improve the visual condition of the urinary bladder, helping to examine and diagnose more accurately and in earlier stages.
- It is helpful to locate even smaller, flat tumors, which are sometimes missed out on traditional cystoscopy.
- Bluelight Cystoscopy is beneficial for removing the tumor during the examination procedure.
- The accuracy rate is much higher than white-light cystoscopy due to accurate cell targeting.
- Low rate of cancer recurrence.
What is the most common symptom of suspected bladder cancer?
Hematuria (painless blood in the urine) is the most common symptom of bladder cancer.
READ SIMILAR: What is the difference between UTI and Bladder infection?
Can blue light cystoscopy work on all types of bladder cancer?
- The mystery of bladder cancer falls into two primary classes,
- About 65 to 70% of bladder cancers fall in the class of NON-MUSCLE INVASIVE BLADDER CANCER (NMIBC), in which the tumor develops in the inner lining of the bladder but does not metastasize deeper into the muscular layer. Doctors considered NMIBC or type 1 as early or superficial bladder cancer.
- Blue light cystoscopy is highly responsible for detecting NMIBC or type 1. As it starts to spread but does not fully spread to other layers, it is a little bit difficult to distinguish from the healthy tissues. At this point, BLC performs its ability very well and helps to diagnose the tumor.
- When we are talking about MUSCLE INVASIVE BLADDER CANCER (MIBC), as the name indicates, it is a rare and more advanced stage of bladder cancer in which the tumor metastasizes into the muscular layer. At this stage, BLC does not work alone. It always works simultaneously with other diagnostic tools like biopsies and imaging methods.
How does blue light cystoscopy coordinate TURBT?
- The identification of suspected bladder lesions is done through positive cytology and cystoscopy.
- When discussing bladder cancer confirmation, doctors use a technique called Transurethral Resection Of Bladder Tumor (TURBT).
- In this procedure, the doctor removes the tumor through the urethra, but remember it is done in the case of NMIBC.
- This sample is examined under a microscope, and the tumor staging and grading are done.
- Blue light cystoscopy is a vital tool to enhance the TURBT.
- During TURBT, blue light facilitates the process by enhancing the cancerous cell to pink so that the doctor more conveniently removes it.
- It is also proven that the coordination of TURBT and BLC lowers the recurrence rate and progression.
Whose are appropriate for blue light cystoscopy?
- Patients who are suspected of non-muscle invasive bladder cancer (NMIBC).
- Patients with positive urinary cytology and no precise tumor detection in white light cystoscopy.
- Doctors require more knowledge regarding bladder lesions to facilitate the treatment scheme.
- To check the tumor recurrence.
- Need of cystoscopy for the first time.
Anesthesia for blue light cystoscopy?
Usually, patients require spinal anesthesia to reduce the discomfort of the procedure. In this case, IV sedations work better as compared to oral administration. The doctor always decides the dose and the combination given to the patient depending on the gender, overall health, and disease progression. But if we are talking about an overall scenario, Midazolam and Diazepam are widely used.
What is the procedure for the blue light cystoscopy?
- At least one hour before the procedure, a catheter tube is inserted into the bladder via the urethra, introducing the contrasting dye solution.
- The cancerous cells absorb the Cysview and illuminate once exposed to the blue light.
- In the initiation of the Bluelight Cystoscopy, patients receive guidelines about how to prepare for the procedure. The doctor will give anesthesia or sedation, usually spinal anesthesia administered through IV, to ensure the patient will be comfortable during the process.
- Once the patient is ready, the doctor gently inserts the cystoscope into the bladder. The doctor initially investigated the bladder with a regular white light cystoscopy to find the lesions.
- Later, the blue light is turned on, illuminating the inside of the bladder to find any spot or area that shows pink, which remains unidentified in the regular cystoscopy.
- The specified lesion is examined or resected for further study.
What is the safety lineage for blue light cystoscopy?
- Any medical procedure or equipment that comes into the hospitals to serve the patients undergoes a long journey of trials and experimentations, so the studies suggested that the blue light cystoscopy is safe and permissible for the patients.
- However, it is also true that every surgical procedure has its side effects, so in this situation, the doctor will decide who will need to prescribe the procedure and why.
What are the possible side effects of the blue light cystoscopy?
The side effects of blue light cystoscopy are the same as those of white light cystoscopy, including:
- Hematuria
- Bladder pain
- Bladder spasm
- Dysuria
The maneuver of BLC in the determination of NMIBC:
- NMIBC is known for its high recurrence rate and progress, so it requires an appropriate identification and exact resection to avoid metastasis.
- WLC has limited outcomes for diagnosis, while BLC contributes to differentiating the areas of malignancy from physiological tissues.
- The complete picture of urine cytology, cystoscopy, and TURBT is crucial for diagnosing bladder cancer.
- The initial stages of bladder cancer with NMIBC are classified as Ta, T1, and carcinoma in situ (CIS).
- Because of papillary identification, Ta and T1 are the initial stages with negative urine cytology and viable tumors in TURBT.
- CIS is more difficult to visualize on TURBT as well as positive cytology. It has rapid progression.
- Cystoscopy and TURBT were performed along with the usual WLC, having a restricted ability to identify the annonemous lesions. This limitation also leads to incomplete resection during TURBT and a high recurrence rate due to the regrowth of remaining or unidentified cells left behind.
- To overcome this, BLC is an advanced technology with photosensitizing fluorescence that can detect bladder tumors better than WLC.
- Malignant tissues possess aggregation of heme precursors. When the hexyl-aminolevulinate (Cysview), a lipophilic precursor of heme, this molecule goes to the urothelium cytoplasm and takes part in heme synthesis.
- The abnormal cells of the malignant tissues have an amassment of protoporphyrin iv in the mitochondria, whereas normal urothelium releases the drug.
- During BLC at an optimum wavelength of 380- 450nm, the porphyrin of malignant cells emits red fluorescence and appears pinkish red, while the healthy cells remain blue.
- This will facilitate the doctor in the accurate identification and removal of tumor clusters, which reduces the recurrence rate.
Conclusion:
In the world of urology, Bluelight Cystoscopy is a brilliant example of how technology can enhance medical diagnosis and treatment. A more transparent view inside the bladder helps doctors catch issues early, improving patient outcomes. So, if you or someone you know is facing bladder-related concerns, remember that Bluelight Cystoscopy is here to shed light on the path to recovery.


1 thought on “Shedding Light on Blue light Cystoscopy: A Revolutionary Tool in Diagnosing Bladder Conditions”