Introduction
Definition of Tubular Secretion:
The nephrons in the kidneys are responsible for monitoring and extracting harmful materials from the blood that are no longer needed in the body; instead, if these waste substances are retained in the body, they will begin to cause pathological disturbance in the body.
Tubular secretion is one of the phases of the filtration process to eliminate such unwanted materials in the form of urine. The nephron performs this function through 3 steps which are:
- The glomerular filtration.
- The tubular reabsorption.
- The tubular Secretion.
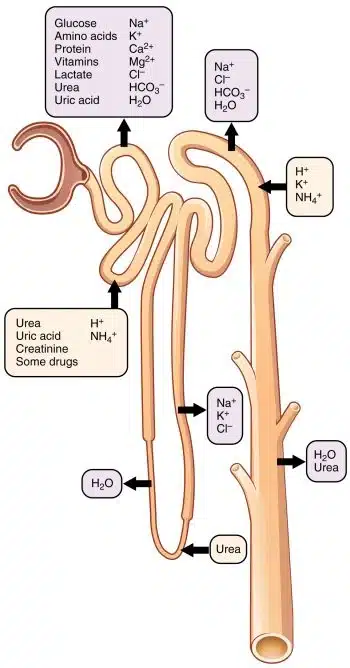
Tubular secretion transfers unwanted drugs, poisons, toxins, and other ions (H+) from blood (peritubular capillaries) to the renal tubule’s lumen through different transport mechanisms. The process is the opposite of tubular reabsorption, where essential substances like glucose, amino acids, and electrolytes move from the tubular lumen back to the bloodstream.
Importance of Tubular Secretion in Human Physiology:
The filtration process, including tubular secretion, is essential in maintaining homeostasis and the acid-base environment of the body. The nephron is specifically designed to adjust the movement of excessively present ions in the body and modulate urine composition.
The tubular secretion also plays a crucial role in maintaining acid-base balance electrolyte concentrations and clearing substances from the bloodstream that are not adequately filtered during glomerular filtration. This selective transfer of substances ensures the disposal of unnecessary materials or ions like urea or uric acid, which had been reabsorbed earlier. This will cause regulation of systemic parameters and is integral to overall homeostasis in the human body.
The tubular secretion will cause the elimination of excessive potassium ions. It also contributes to The regulation of the pH of the blood. If the blood pH is towards an acidic medium, kidneys secrete more H+ ions into the filtrate and conserve more HCO3 to neutralize the environment.
The significance of tubular secretion lies in its contribution to the meticulous control of ensuring our internal systems run smoothly and keeping our bodies in optimal working condition, highlighting its indispensable role in human physiology.
Little explanation of the Nephron Structure:
Before understanding the process of tubular secretion, it is necessary to know some basics of nephron anatomy to determine renal physiology more easily. The nephron is divided into two parts, which are:
Renal Corpuscle:
- It is the initial part of the nephron responsible for the duty of blood filtration. It consists of Bowman’s capsule and the glomerulus.
- Bowman’s capsule comprises the outer parietal layer and the visceral layer. The visceral layer is lined with the podocyte, with foot processes covering the glomerular capillaries.
- The glomerulus is the network of capillaries emerging from afferent arterioles and ending at efferent arteriole. The capillaries are lined with endothelial cells as well as mesangial cells.
- This is the site where the blood filters; during this filtration, various particles, either essential or non-essential, become added to the filtrate from the blood with the help of the glomerular basement membrane. The overall process depends on the particle’s size and charge having on it.
Renal Tubule:
- It is the next portion of the nephron, consisting of a long pipe-like structure next to the renal corpuscle.
- It is further divided into (1) the Proximal convoluted tubule, (2) the Loop of Henle, (3) the Distal convoluted tubule, and (4) the collecting tubule.
- The loop of Henle is further divided into the descending limb of the loop and the ascending limb.
Substances that are secreted out from tubules:
The secretion process usually drains out those more bulky substances to be filtered or excessive in blood. The substances which are secreted from the bloodstream toward the filtrate include:
- Potassium ions (K+)
- Hydrogen ions (H+)
- Ammonium ions (NH4+)
- Creatinine
- Urea
- Some hormones
- Some drugs (e.g., penicillin).
”SECRETION VS EXCRETION” 8 POINEER POINTS TO REMEMBER!
Sites specifically for tubular secretion:
The proximal convoluted tubule is the primary site for tubular secretion except for potassium ions. Simultaneously, some ions become secreted in the cortical region of the collecting tubule and the later distal convoluted tubule.
Mechanism of Tubular Secretion:
Secretion at Proximal convoluted tubule:
- The process of tubular secretion works in coordination with tubular reabsorption. The filtrate from the renal corpuscle differs from blood regarding R.B.C.s and large proteins. When this filtrate reaches the tubular system (proximal convoluted tubule), various modifications occur in secretion and reabsorption until the final product (urine) is formed.
- Most ions move across the proximal convoluted tubule’s membrane either through reabsorption or secretion. After the deamination process of amino acids occurs in liver hepatocytes, ammonia (a by-product of protein metabolism) formed and secreted into the P.C.T. lumen simultaneously Na+ and HCO3- transport toward the interstitial fluid of kidney pyramid through symport transport (2 or more molecules move toward the same direction).
- During this process, there is a net loss of H+ ions, which combine with the ammonia to form a weak acid NH4 in the urine; at the same, there is the gain of bicarbonate ion (HCO3-) transport toward the blood.
- The ammonia and bicarbonate exchange ratio is 1:1. This is how the body excretes acid and maintains the blood pH.
Secretion at Loop of Henle:
- As discussed earlier, ammonia is a toxic end product formed due to amino acid deamination, in which the amine group is removed. A large quantity of ammonia is converted into urea.
- Urea is a less toxic by-product, and kidneys handle urea more efficiently. At the Loop of Henle, more specifically at the descending limb of the loop of Henle, various aquaporin channels are found, which facilitates the free diffusion of water into the interstitial space along with the diffusion of urea into the lumen of the descending loop.
Secretion at Distal convoluted tubule:
- As the filtrate enters a distal convoluted tubule, a tremendous amount of water is present in the filtrate, so at this portion, aldosterone regulates the secretion/reabsorption of water molecules by enhancing the activity of Na/K ATPase.
- Cells of the D.C.T. have parathyroid hormone receptors responsible for the secretion or reabsorption of Ca++ ions. When the parathyroid hormone molecules bind with these receptors, it opens calcium channels at the luminal surface. So, the calcium is returned from the almost-formed urine.
- There is also a contribution of Na+ coming out of the cell. Hence, an electrochemical gradient is formed, which attracts Ca++ inside the cell. If sufficient PTH receptors are not found due to aging or vitamin D deficiency, the Ca++ is not reabsorbed and secreted in the urine.
Secretion at collecting ducts:
- The process of secretion that occurs at the collecting ducts is specifically dependent upon the osmolarity of the body. Suppose the blood is hyperosmotic, which means the blood is more viscous, and the water concentration decreases. In that case, the collecting ducts conserve more water to dilute the blood (reabsorption process), which results in more concentrated urine.
- Similarly, if the plasma osmolarity declines, the blood is less viscous, and the water concentration is high, increasing blood volume and blood pressure. In this case, low or no water reabsorption and secretion of water molecules occur in the urine. The urine is less concentrated.
- The above process of reabsorption and secretion is regulated through the antidiuretic hormone (ADH) secreted by the posterior pituitary gland.
- If the body feels dehydrated, the plasma osmolarity is high, detected through the osmoreceptors found in the hypothalamus, stimulating the ADH release. Various aquaporin (water-loving) channels are in the collecting duct’s principal cells.
- ADH stimulates these aquaporin channels; water will attract toward these channels through osmosis from collecting ducts toward interstitial spaces and finally toward the peritubular capillaries. So, the plasma osmolarity returns to normal.
- If the body is overhydrated or has no dehydration, ADH release declines, fewer aquaporin channels work, and less water moves toward the peritubular capillaries, producing more water secretion and diluting urine.
Impact on Blood Pressure and Fluid Balance:
- The entire process is not only regulated through ADH; rather, it is influenced through the release of aldosterone. Aldosterone is a steroid hormone released through the adrenal gland in response to activation of R.A.A.S. (renin-angiotensin-aldosterone-system). It is an essential hormonal system that regulates blood pressure through blood volume and fluid balance.
- The principal cells of collecting ducts also have receptors for aldosterone. Aldosterone is primarily required for Na+ reabsorption. In the body, when there is low blood pressure, R.A.A.S. activates and induces the receptor for Na+ reabsorption from the lumen by activating Na+/K ATPase.
- As a result, more Na moves toward the body, and water follows it from the urine. Simultaneously, K moves from the body toward the urine as both move in opposite directions. This will induce high blood volume, maintaining blood pressure and decreasing urine volume.
- The exact mechanism occurs in reverse in the case of normal/low blood pressure—no activation of R.A.A.S. secretion of Na plus water in urine and K reabsorption in the body.
Conclusion:
In conclusion, a comprehensive understanding of tubular secretion is vital for unraveling the intricacies of renal physiology and the overall functioning of the urinary system. Tubular secretion, a pivotal process in the nephron, involves:
- The active transport of substances from the blood into the renal tubules.
- Contributing significantly to the regulation of electrolyte balance.
- Acid-base equilibrium.
- The elimination of waste products.
This intricate mechanism plays an essential role in maintaining homeostasis within the body. By meticulously examining tubular secretions, researchers and healthcare professionals can enhance their grasp of renal function and develop targeted interventions for conditions associated with impaired tubular secretion. As ongoing research continues to identify the complexities of this process, a more profound comprehension of tubular secretion promises to advance our knowledge and pave the way for innovative approaches in the diagnosis and treatment of renal disorders.
F.A.Q:
What is the difference between tubular secretion and excretion?
The significant difference between tubular secretion and excretion is that tubular secretion removes specific molecules from the body into the urine. During urine formation, depending upon the body’s state of osmolarity, the kidney defines which substances need to be secreted and which must be reabsorbed.
Tubular excretion is a generalized term used when diffusible molecules move from peritubular capillaries toward the lumen of the renal tubule favored by a concentration gradient.
What is the tubular secretion of proteins?
It is the capability of the tubule system, specifically the proximal tubule, to remove unfiltered and retained solutes and drugs, which are usually protein-bound, so they cannot filter the glomerular filtration membrane because of the size and charge specification.
What is the acid tubular secretion?
The acid tubular secretion is the renal mechanism for maintaining the acid/base balance of the body with the help of recovering/releasing H+ or HCO-3 into the forming urine. This process specifically occurs at the renal tubule and solely depends upon the pH of the blood. If the blood pH drops, the kidney releases more H+ (acid) into the urine and vice versa.
Why is tubular secretion an active process?
Yes! Tubular secretion is an active process with a carrier-mediated transport system that requires ATPase for molecule transport.
What is the difference between tubular secretion and reabsorption?
Tubular secretion transports solute or water molecules from the peritubular capillaries toward the interstitial space and into the tubular lumen. These are the molecules that are no longer needed by the body. At the same time, tubular reabsorption is the movement of molecules from the renal tubule toward the body through peritubular capillaries. With this process, the body recovers essential molecules back into circulation.
What is a tubular secretion in urine formation, in simple words?
In the process of urine formation, tubular secretion is the process of adding solute or water molecules into the urine, which is no longer needed by the body, and these molecules escape earlier from the glomerular filtration process.
What are the two main sites of tubular secretion?
The proximal convoluted tubule P.C.T. and distal convoluted tubule D.C.T. are two major sites for the secretion process.
Is tubular secretion part of urine formation?
Yes, of course! Tubular secretion is an integral and vital phase of urine formation by which the concentration and volume of urine are adjusted.
References:
https://courses.lumenlearning.com/suny-ap2/chapter/tubular-reabsorption-no-content/
https://biologydictionary.net/tubular-secretion/
images are taken from:
25.5 Physiology of Urine Formation: Tubular Reabsorption and Secretion
3 thoughts on “What is Tubular Secretion? Discover the Secrete Code of Fluid Balance!”